Pain Relief - is there another way?
We read in a report this month from Public Health England, that nearly 12 million people – about one in eight adults in England – are taking medicines for pain, depression or insomnia, which they can find hard to stop.
Shockingly, half have been on these medicines for a year or more and more than a fifth for over three years. Prescribing rates are 1.5 times higher for women than for men.
There may be good reasons for people to use antidepressants over a long period, but the widespread prescribing of opioid painkillers, benzodiazepines and sleeping pills needs to change, the review says. GPs should instead consider social prescribing, from talking therapies to joining a club or social group activity, like a choir.
Painkillers like ibuprofen, Paracetamol, also known as acetaminophen, and in increasing numbers, opioids, have become our go-to solutions for pain management. Opioids - such as codeine phosphate, tramadol, morphine, fentanyl and oxycodone, in particular, are often hailed as the holy grail in pain relief and management but come at a price - nausea, drowsiness, GI symptoms, especially constipation, addiction and abuse.
Many herbs and spices have anti-inflammatory properties that can provide pain relief which I want to provide for you, but first let me explain what inflammation is.
What Is Inflammation?
The inflammatory process is a vital and necessary component of our immune defence system. It aims to remove harmful or foreign invaders and heal itself. Without inflammation we wouldn’t survive very long! When immune responses are temporary and local, the inflammatory process is beneficial. However, when the regulation of inflammatory responses breaks down, they can result in processes that actually can lead to the damage of tissues and organs - a hallmark of chronic dis-ease. This break down of immune regulation can manifest as more outward signs of redness and swelling, pain and /or autoimmunity.
In terms of pain management, the most commonly targeted enzyme pathway for drug therapy are the family of enzymes that facilitate the production of proinflammatory mediators. These enzymes are called Cycooxyengase and lipoxygensase, more commonly referred to as COX & LOX, and the drug therapy then are COX & LOX inhibitors (hope you are still with me!).
Explaining how the Inflammatory pathway to pain plays out
1. The inflammatory pain pathway begins with the trigger, which could be:
Injury to a barrier like the skin,
An infection, a bacteria, a virus, mould, pollen that docks onto a receptor on the outside of a cell membrane and kick starts the chain reaction to follow,
A food protein can bind to IgE or IgG antibodies expressed on the cell membrane of genetically predisposed individuals. For example an allergen + IgE + mast cell cross links and disrupts cell membrane of a mast cell, and start the cascade
2. The Cell membrane now becomes become comes permeable to calcium entering the cell which triggers an enzyme (Phospholipase A2) that liberates a pro-inflammatory precursor, Arachodonic acid, from the cell membrane. In the medical world, steroids are used to prevent this occurring, or a natural compound that can inhibit Phospholipase A2 is bromelain.
3. The enzymes COX & LOX act on the now liberated and available Arachidonic Acid to produce pro-inflammatory mediators (prostaglandins, thromboxanes and leukotrienes). These mediators manifest themselves as itching, vasodilation etc and also induce the production of inflammatory communication molecules called cytokines - a whole inflammatory storm now starts brewing.
These cytokines: interleukin-1 (IL-1), tumor necrosis factor (TNF), gamma-interferon (IFN-gamma), IL-12, IL-18 themselves cause pain but also activate the master aka The Terminator, of the inflammatory cascade - NF-κB. Found in almost all animal cell types NF-κB is involved in cellular responses to stimuli such as stress, cytokines, free radicals, heavy metals, oxidized LDL, and bacterial or viral antigens Incorrect regulation of NF-κB has been linked to inflammatory and autoimmune diseases, septic shock, viral infection, and improper immune development. It all becomes a horrible vicious cycle!
Drugs such as aspirin, ibuprofen and paracetamol work by blocking COX enzymes but have negative side effects, namely thinning of gut mucosa aka, intestinal permeability, and thus when overused results in many gut related symptoms.
The most common LOX 5 inhibitor drug is Diclofenac. Side effects written on this medication’s box are Diarrhoea, gastrointestinal irritation and abdominal pain - nice!
4. Other immune reactions are that mast cells degranulate and release histamine which typically is thought of in allergies, but also I see plays a part in reflux, IBS-Diarrhoea type, migraines and heartburn. And, the formation of immune complexes:
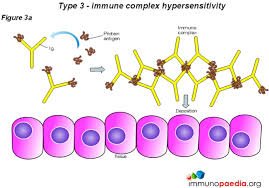
An immune complex, sometimes called an antigen-antibody complex, is a molecule formed from the integral binding of an antibody to a soluble antigen. Immune complex deposition is a prominent feature of several autoimmune diseases, including systemic lupus erythematosus, rheumatoid arthritis, scleroderma and Sjögren's syndrome.
What natural compounds can we use?
LOX inhibitors: boswellia and curcumin. I use these products BCQ by Vital Nutrients and TurmaForte by Wild Nutrition
COX inhibitors: quercetin, nettle and butterbur
Immune complexes: systemic enzymes and Boswellia, A clinical trial conducted in 2008 found that boswellia significantly improved arthritic pain and joint function in as little as seven days. Other studies suggest that the anti-inflammatory effect of boswellia is comparable to that of ibuprofen. Phyto-Curcumin Plus Enzymes by Vital Nutrients contains Curcumin Phytosome Extract, Bromelain, and Serratiopeptidase. I recommend 2 capsules twice a day away from food by at least an hour.
And no conversation about inflammation is complete without mentioning omega-3 fatty acids. The downstream metabolites - EPA and DHA support the body’s inflammatory response across multiple areas of the entire inflammatory response. I recommend Lion Heart liquid or Maxi Caps if you don’t like a liquid, by Bare Biology. I would recommend 2-3g a day (1tsp of the liquid= 2g).
As always, in health, Tanya x