IBS: from top to bottom
The Gastrointestinal tract, or “gut” as it is more commonly termed has may roles and mechanisms.
When assessing clients that come to see me with functional digestive disorders, rather than focus on what specific disease they may or may not have, I endeavour to assess and restore normal function across all the digestive process, which is best broken down into 5 areas of function.
The 5 key roles of the digestive system:
Digestion & absorption
Immune function & Oral Tolerance
The Gut microbiome
The maintenance of an immune barrier
The Nervous system of the gut
All too often with symptoms of more classic gut symptoms such as bloating, distension, gas and reflux, we are heading straight to the microbiome with the blanket statement “treat the gut” and not thinking about what mechanisms are at play. Simply ordering a stool test, recommending a probiotic or antimicrobial and some glutamine to heal intestinal permeability is not going to work if, for example, the vagus nerve, aka enteric nervous system is involved, or the digestive secretions:- HCL, pancreatic and brush border enzymes are deficient or indeed if there is a sluggish gall bladder. An assessment across all 5 areas of the GI tract needs to be made before planning an intervention.
Firstly, as we assess digestion in the stomach, the key thing is to have sufficient acidity to digest proteins as well as being antimicrobial in nature. If you feel as if a brick has hit your stomach after eating a protein-rich meals or you don’t like to eat really high animal protein meals because you feel distended or bloated then that suggests there is a hydrochloric acid deficiency issue. In people that aren’t producing hydrochloric acid, they lose the ability to break down their protein, the protein goes through a putrification process and that creates more burning, and so they get this paradoxical reflux pattern, even though they’re actually low on hydrochloric acid!
The most common causes of low hydrochloric acid are:
Helicobacter Pylori infection
Hypothyroidism
A traumatic brain injury
Medications
Dysautonomia
Brain neurodegeneration
Which obviously in a functional approach, are assessed and addressed.
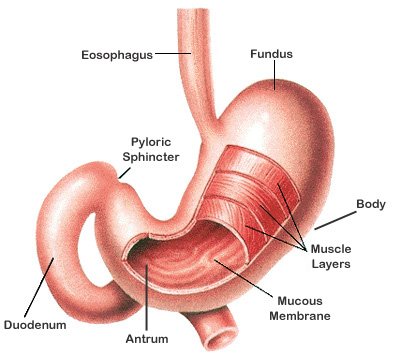
A note on Helicobacter Pylori here: initial overgrowth and colonisation with H.Pylori (exposure to which is chronic for most of us) is in the body of the stomach and there it infects the cells that produce HCL, causing hypochlorhydria and this can last from 3-up to 24 months with no symptoms of gastritis or ulcers, but causing a low HCL output. A low HCL output places us at a much higher risk of developing SIBO and other gut infections.
Signs & Symptoms of Low HCL are:
Gas, bloating and burping
Constipation
Feeling of fullness or food not digesting
Bad breath
Foul smelling stools
Loose stools in the early morning
Food sensitivities
Progressively the infection moves from the body of the stomach to the antrum where it has an effect on increasing gastrin output- specifically gastrin17 which increases acid production and has a negative impact on Somatostatin. In the gastrointestinal tract, somatostatin reduces gastric secretion.
The best testing for H.Pylori is either a breath test or stool antigen test for an active infection.
A low HCL will very quickly have a knock-on effect onto the pancreas exocrine function as the production of enzymes from the pancreas is dependant upon HCL production. On a stool panel elastase is a robust marker for pancreatic exocrine function. Levels of 350 or less, hypochlorhydria is likely.
The other digestion secretion to consider is the gall bladder, a form of biliary stasis, like a pre-gallstone state, translates into inadequate release of bile into the small intestine and this can have a number of impacts:
Bloating and burping after meals
Low intolerance to fatty foods
Microbiome imbalance and signalling (due to low bile salt synthesis)
Sometimes, if you have had your gallbladder removed the cystic duct then just pouches into a new gallbladder and you can be prone to have issues with fatty food digestion.
So, just in this post, all I've done is go through the first section - Digestion, and we can see how important a thorough assessment is when working with IBS.
if you are a client - I’ll be sharing all this knowledge and much more in bite-size, usable data at my Functional Gut Day Retreat on 9th October - only 3 spots left - if this resonates, book now!