SIBO & Motility The Tide is High & I’m Holding On!
In the words of Debbie Harry…… “The tide is high” and with regards to SIBO the landscape of this condition is most certainly…. moving on, rather than holding on!
There have been a couple of areas that I have delved into recently, and wanted to take some time to explain.
Firstly, What is SIBO
The definition of SIBO is a condition in which abnormally large numbers of bacteria and/or archaea are present in the small intestine, leading to impairment of digestion and absorption as well as systemic inflammatory effects.
Normally, bacteria are found in their trillions in the Large Intestine, where they perform numerous symbiotic functions for our overall metabolism. The small intestine is supposed to have less than 10 CFU/mL of bacteria. The large intestine, by contrast has significantly more - 1011 microbes/mL .
When present in the small intestine in larger amounts, these bacteria are then able to act on poorly digested, fermentable carbohydrates producing hydrogen gases, which results in symptoms such as bloating, gas, abdominal pain, diarrhea and/or constipation. Other organisms termed Archea, naturally present in the small intestine, can also use the hydrogen produced to make methane gas.
The effects of SIBO can extend beyond direct gastrointestinal symptoms. Increased gut permeability can occur, causing translocation of bacteria and insufficiently digested food particles that trigger immune activation. This can lead to pain and other symptoms such as brain fog, and also predisposes an individual to food sensitivities.
Nutrient deficiencies can arise as the bacteria consume some of the ingested foods, for example B12 and iron, which can lead to anemia and the deconjugation of fatty acids from bile, which reduces absorption of fat-soluble vitamins, A, D, E and K.
Small Intestinal Bacterial Overgrowth (SIBO) is actually a very common (up to 84%) yet often undiagnosed cause of Irritable Bowel Syndrome (IBS).
Symptoms of SIBO are:
Bloating and Gas
Belching & flatulence
Abdominal Pain & Cramps
Constipation & Diarrhea
Heartburn
Nausea
Systemic symptoms : food sensitivities, h/a, joint pain, respiratory, skin, brain fog.
Malabsorption Symptoms: steatorrhea, anaemia and low vitamin D
Preventing SIBO Occurring
We do have built in mechanisms to prevent bacteria overcrowding the small intestine.
Firstly “Digestive Secretions”:
Hydrochloric acid or stomach acid plays many roles, one is to sterilise food that has been consumed and as part of our first line of defence eradicate “incoming” bacteria from the oral cavity and mouth. Thus, if stomach acid is low then excess bacteria could colonise the small intestine. Being on a PPI (which decreases stomach acid production).
Pancreatic, Brush Border “digestive” enzymes and bile all aid in the digestion process of food in the forms of protein, carbohydrates and fats. An impairment in this process provides more substate to ferment
Secondly:
The gut mucosal immune system (MALT) attacks foreign pathogens and regulates the commensal probiotic bacteria
And the final one - is hugely significant as it relates to SIBO and the immune system:
The migrating motor complexes. Migrating motor complexes (MMC) are waves of electrical activity that sweep through the intestines in a regular cycle during fasting
The MMC sweeps any undigested food & organisms towards the ileum (the last portion of the small intestine and the ileocecal valve - the gateway into the colon/large intestine. In adult humans, the small intestine is usually 6-7m long.
Between meals this reflex sweeps a “peristaltic” wave from the stomach to the ileum every 90 minutes. It stops when taking in any “calories” - even stevia has been shown by Dr Mark Pimentel (an expert on conditions related to the microbiome, including small intestinal bacterial overgrowth) to cease the MMC.
Anything that decreases the MMC increases the “risk factor” of developing SIBO.
Now we understand this, there are certain chronic systemic conditions that can cause motility issues and would most certainly be a risk factor and /or predispose an individual for developing SIBO:
Diabetic neuropathy to the Autonomic Nervous System (ANS), particularly in the gastrointestinal tract (GIT)
Scleroderma - a group of diseases with a common symptom: hardening and tightening of the skin or connective tissue disorders such as Ehlers–Danlos syndrome (EDS) which causes loose joints, joint pain, stretchy or “floppy” collagen and abnormal scar formation
Gastroparesis - a disease in which the stomach cannot empty itself of food in a normal fashion.
Hypothyroidism - a condition that slows the metabolic rate of potentially every cell, including gastrointestinal cells.
In addition structural or anatomic abnormalities may affect normal movement of the small intestine (motility). This can occur if you:
Have diverticulosis — tiny bulging pouches (diverticula) in the small intestine
Had surgery that changed the small intestine’s structure, such as Roux-en-Y gastric bypass surgery, or surgery on the right colon with removal of the ileocecal valve, or surgery on the last part of the small bowel.
Have adhesions (scar tissue) that developed after radiation therapy or after multiple abdominal surgeries or endometriosis
Have amyloidosis (a buildup of amyloid protein deposits) — deposits can accumulate in the small intestine and change its structure
The other category of most likely underlying cause is an immune reaction following a case of food poisoning, traveller’s diarrhea or gastroenteritis:
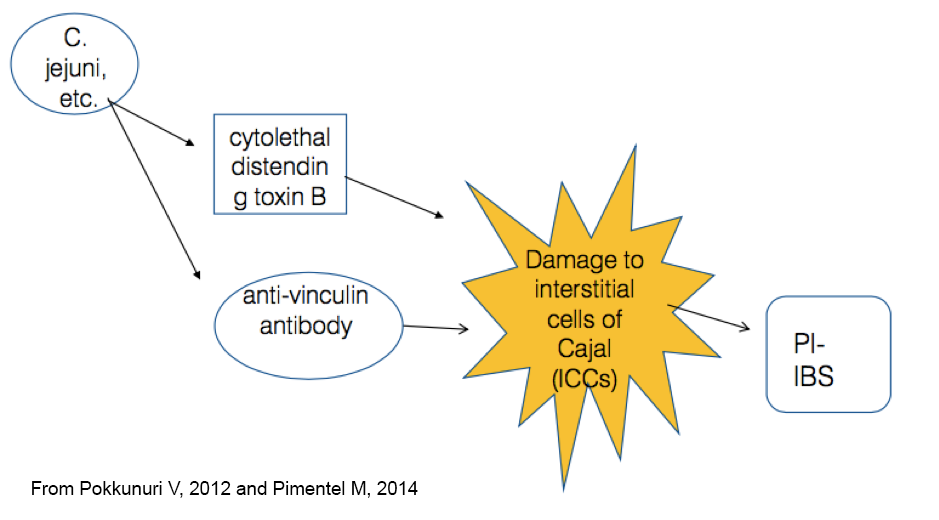
Bacteria that are the main culprits for such events, E.coli, Salmonella, Shigella and Camplylobacter jejuni, produce a very strong toxin called cytolethal distending toxin (CDT). When these toxins are encountered the immune system produces antibodies against them as a function of defence - so far so good. However, CDT antibodies appear to have a strong affinity to the interstitial cells of Cajal and ganglia (part of the MMC) and in essence mount an “attack” against self tissue, affecting gut motor function.
To add insult to injury, due to the “antigenic similarity between CDT and intestinal, cytoskeleton (basically the internal scaffolding of gut cells) proteins such as talin and vinculin, a further attack occurs to this ”scaffolding” and thus lays the groundwork for further structural abnormalities..
What can we do to aid the action of MMC & Misconception No1
The use of a Prokinetic here can be very helpful. A prokinetic is an agent that by definition can amplify and co-ordinate gastrointestinal motility
And here comes misconception No 1 , that a prokinetic produces a bowel movement - it doesn’t. The motilities of the small and large intestines are independent of each other. Bowel movements are not related to the MMC. A laxative and a prokinetic have different areas of focus.
A Prokinetic amplifies and co-ordinates the downward movement of the different segments or chambers of the GI tract. For example, in terms of the stomach: - to open the lower pyloric sphincter and close the upper lower oesophageal sphincter.
And then of course to amplify and stimulate the MMC to clear bacteria from the small intestine.
A prokinetic could affect the large intestine, but to affect the large intestine would need to be at much higher dose and is not really it’s primary role.
Types of Prokinetics
3 are pharmaceutical, so you’ll need a prescription from a specialist doctor
Low dose erythromycin (an antibiotic)
LDN
Prucalopride
Or herbal combinations that contain ginger root or ginger containing formulas which has been shown to have very effective prokinetic affects: I use Bio.me Kinetic
A laxatives role (details at the end on what type of laxatives I use) then is to produce a bowel movement in the large intestine and does not have a prokinetic affect at all - they do not stimulate the MMC.
Bowel movements are not related to the MMC but by contractions or mass movements (occurring up to 6 x a day) triggered by gastrocolic reflexes.
The gastrocolic reflex is a reflex that stimulates contractions in the colon, that can lead to a trip to the toilet shortly after eating a meal. Basically the stomach and the colon are communicating – once the food you have just eaten reaches the stomach, the stomach sends a message to the colon to make room because more food is coming. The colon starts contracting which pushes its contents further down and this is why you have a bowel movement - often shortly after you have eaten a meal. It’s not the food that you have just consumed, it’s waste from food that you had eaten earlier that was already further down in the digestive tract.
Research has shown that some patients with IBS have an over-reactive gastrocolic reflex with high pressure contractions in response to meals. Simply eating or drinking can trigger this exaggerated reflex resulting in pain, cramping, diarrhea or constipation.
The wonderful herb camomile seems to help in this situation of an over-reactive gastrocolic reflex, and loose stools. Pukka herbs do a lovely camomile herbal tea, and this product in my experience works wonders IB Pro
Tips to help the upper digestive secretions “flow” and thus act as a preventative
Take time over your meals, chewing and engaging with your food sends messages via the vagus nerve to expect food and to place the nervous system into parasympathetic mode - ready for rest and digest!
Having some apple cider vinegar in a little water just at the start of a meal can help with the digestive process
Include bitter greens before or after a meal: rocket, endive, chicory, watercress are good ones readily available in the UK
Consider supplementing with a digestive enzyme complex
Digest Select: is a comprehensive, broad-acting digestive enzyme complex intended to help support and promote the proper breakdown of food. The formula contains amylase enzymes that help digest simple and complex carbohydrates, protease enzymes that help digest proteins and peptides, and lipase enzymes that help digest fats. Lactase and alpha-galactosidase enzymes are added to help support the healthy digestion of milk sugar (lactose) from dairy foods, and complicated starches such as those found in beans, grains, and cruciferous vegetable
Or Digestzyme, which is comprised of a proprietary blend of digestive enzymes along with the addition of Betaine HCL to support optimal digestion of proteins, fats, and carbohydrates. This product also contains the special protease DPP IV (dipeptidyl peptidase IV), which aids in the breakdown of the peptides gluteomorphin (from gluten) and casomorphin (from casein).
Or a Bitters formula: Dr. Shade’s BitterX is a formulation of supporting bitter compounds: Extracts of Dandelion (root), Gentian (root), Solidago (aerial parts), and Myrrh (Oleo-gum-resin), using Quicksilver Scientific’s patented liposomal delivery form for higher-than-normal bioavailability and absorbability.
Different Forms of laxatives
As always, I would work on the underlying cause of why an individual is not producing a regular bowel movement, but here is information that can help provide some symptomatic relief.
Osmotic laxatives are based on larger molecules that are poorly absorbed and thus draws water into the lumen. Common ones are magnesium citrate or oxide. They take a couple of days to work and you need to find your “sweet spot”. 800mg seems to be a common “sweet spot”, take at bed-time and away from food by at least 2 hours, and it can take 2 -3 days to have an affect.
Movicol is often prescribed for children - which I don’t really like as it’s not a natural product. What is helpful for children (in fact I have been using this with success with a great friend of mine’s daughter who has Downs Syndrome and as such has a natural propensity to constipation) is papaya. Caricol®* is an entirely natural organic product made from the pulp of tree-ripened papaya, and can be purchased here
For adults, my favourite combination of magnesium oxide with Triphala, an Ayurvedic herb is Colon Rx™. Magnesium hydroxide is a well-known ingredient in laxative and antacid formulas, while Triphala is a classic formula in Ayurvedic medicine.
It can be used for short periods of time as a fast-acting mild laxative for occasional constipation, or as a daily bowel tonic to help strengthen and unify the bowels. I would start with 2 capsules at bedtime.
Stimulatory laxatives
These work by stimulating the muscles in your bowel to contract more often and with more force, like Senna and cascara . These work more quickly but are more agitating and more associated with cramping in my experience.
Serotonin (or 5HT) agonists
Such as prucalopride (at a higher dose than is prescribed for it’s use as a Prokinetic). This type of medicine causes your bowel muscles to contract. You’ll need a prescription from a specialist doctor for this.
In health, Tanya x
In part 2 of this post I discuss misconception No 2 in the world of SIBO. Colonic bacteria has an opportunity to migrate from the colon to the small intestine……… this may well not be the case!