Myth Busting Adrenal Fatigue & Cortisol Steal!
Have you been told or bought into any of these statements ?
You have adrenal fatigue!
“You are suffering as a result of “cortisol steal” - it’s hijacking/ stealing away from all of your other hormones, such as oestrogen and DHEA
Your adrenal glands are your back up at peri menopause and menopause
All these statements are incorrect. “Adrenal fatigue”, “adrenal exhaustion” and cortisol steal - are terms offered as a “diagnosis” by sadly too many practitioners to summarise the complex dysfunctions related to the stress response.
It’s true, that “stress” does manifest clinically other than in extreme conditions such Addison’s disease or Cushing’s disease but using terms as adrenal fatigue and explanations such as cortisol or pregnenolone steal as a mechanism for “stealing” away to the detriment of other hormone production, is simply not correct or indeed biochemically possible - let me explain more.
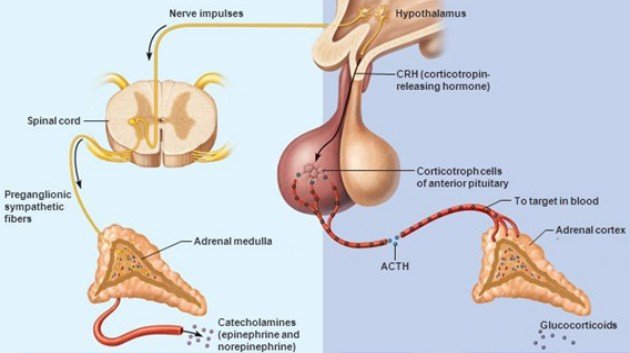
Firstly, let's review the stress response
When you feel stressed, whether you face a real threat or merely think that you are facing a threat, your body experiences a collection of changes known as the stress, or fight-or-flight response. This response is the collection of physiological changes that occur when you face a perceived threat, that is when you face situations where you feel the demands outweigh your resources to successfully cope. These situations are known as stressors.
A stressor can be physical (like running a marathon, coping with inflammation from an infection, or even a latent food intolerance like a sensitivity to gluten) or emotional (like being a new mum, going through a divorce or dealing with conflict at work). This wonderful infographic, adapted from the work of Thomas Guilliams in his book The Role of Stress & the HPA axis in Chronic Disease, beautifully illustrates what stressors are to the master controller of this response - the hypothalamic-pituitary axis.
What Happens During the Fight-or-Flight Response
In response to these stressors, the body's sympathetic nervous system is activated to stimulate the adrenal glands initially triggering the release of adrenaline and noradrenaline, through nerve fibres which is immediate and then approximately 20 minutes later via the HPA Axis and a hormone relay (CRH - ACTH) the Glucocorticoids, namely cortisol and cortisone are released.
These hormones result in an increase in heart rate, blood pressure, and breathing rate. Some of the physical signs that may indicate that the fight-or-flight response has kicked in include:
Rapid Heart Beat and Breathing
Pale or Flushed Skin: As the stress response starts to take hold, blood flow to the surface areas of the body is reduced and flow to the muscles, brain, legs, and arms are increased. You might become pale as a result, or your face may alternate between pale and flushed as blood rushes to your head and brain. The body's blood clotting ability also increases in order to prevent excess blood loss in the event of injury.
Dilated Pupils
Trembling: In the face of stress or danger, your muscles become tense and primed for action. This tension can result in trembling or shaking
After the “threat” is gone, it takes between 20 to 60 minutes for the body to return to its pre-arousal levels.
Beware of the adrenal fatigue ‘diagnosis'
What I was taught at nutrition college and other institutions (sadly) is that the adrenal glands being exposed to chronic stressors can't cope and eventually cease cortisol output - termed adrenal fatigue. This hypothesis is driven by the “theory of pregnenolone or cortisol steal“. While it is correct that all steroid hormones are in fact made from from pregnenolone, which ultimately comes from cholesterol (yes, sex hormones are made from cholesterol!) the hypothesis goes wildly awry, that this elevated cortisol either by acute or chronic stress, leads to less pregnenolone becoming available to be converted to DHEA and other hormones. So, in other words the need for cortisol, "steals" pregnenolone away from the other hormones. Unfortunately, this diagram/ explanation is used to teach steroidogenesis (making of steroid hormones) showing a common pathway - and a common “pool “ of pregnenolone within the adrenal - like this:
And when “stressed” all the pregnenolone is diverted towards the cortisol pathway, to the detriment of the other hormones, such as androstenedione, DHEA and oestrogen. And this is given as a reason, especially for peri- and postmenopausal women as to being a drain on their oestrogen production, as the adrenals produce a small amount post menopause when the ovaries stop.
The truth of the matter is - this is biochemically impossible! There is no such thing as cortisol or pregnenolone steal!
Firstly there are different zones of the adrenal glands that house different enzymes within each of these zones and pregnenolone is stored within the mitochondria of each cell of these zones, as shown here:
Mitochondria cannot and do not steal from each other! And the enzymes required to convert progesterone into DHEA and Oestrogen are only present in the Reteticulus zone - they don’t hop across to another zone!
But I do feel fatigue - What is going on?
The stress / fight or flight response is indeed real and this response is highly effective, fast and generates a vast amount of energy. It also takes priority over other metabolic functions that are deemed non-essential activities in a state of “stress” such as digestion, growth and reproduction. These deemed non-essential process are in essence “put on hold” and therefore don’t function as well and so symptoms and conditions such as hair loss, weight gain, bloating, IBS, reflux, fatigue, PMS to name a few start to occur as different glands (adrenal, thyroid , ovaries) become affected, through a maladaptation of the master controller - the HPA axis. The term then HPA Axis Dysfunction is a much more appropriate term to describe the many consequences that link stress with the myriad of negative outcomes related to the stress response. A reduced HPA axis function can and does result in low cortisol levels which is common in fibromyalgia, chronic fatigue syndrome, PTSD and individuals with high psychosocial “burnout.” The “treatment” for which then should be brain based ( given the hypothalamus and pituitary are brain related) with the use of adaptogens, nervines and phosphatidylserine (I LOVE love love this and by it’s in my brain booster kit - in the Neuro C product). Together with of course, unravelling and removing the many triggers/ or stressors that are literally bombarding this master controller axis, in other words - a root cause approach!
And for the science geeks among you, what then, is true Adrenal Insufficiency?
True Adrenal Insufficiency is a deficient production or action of glucocorticoids - cortisol and aldosterone and has potential life-threatening consequences, because cortisol has many “good” jobs to do:
It controls your blood pressure and your heart rate
It controls how your immune system deals with viruses, bacteria, and other threats
It puts more sugar in your bloodstream to give you more energy
It adjusts how your body breaks down carbohydrates, proteins, and fats
Aldosterone keeps the sodium and potassium in your blood balanced, which helps control your blood pressure and the balance of fluids in your body.
When there’s not enough of these hormones, your body has trouble with these basic functions. That causes the symptoms of adrenal insufficiency - fatigue, muscle weakness, low appetite, weight loss, and pain and belly swelling.
You can have either primary, secondary or tertiary adrenal insufficiency:
Primary adrenal insufficiency is when your adrenal glands are damaged and can’t make the cortisol you need. They also might not make enough aldosterone.This condition is often called Addison’s disease.
Secondary adrenal insufficiency is more common than Addison’s disease. The condition happens because of a problem with your pituitary gland that makes the hormone called adrenocorticotropin (ACTH). This is the chemical that signals your adrenal glands to make cortisol when your body needs it. If your adrenal glands don’t get that message, they may eventually shrink.
Tertiary starts at the beginning in the hypothalamus. It makes a hormone called corticotropin-releasing hormone (CRH) which tells the pituitary to make ACTH. When the hypothalamus is not making enough CRH, then it affects the pituitary’s ability to produce ACTH , in turn keeping the adrenal glands from producing enough cortisol.
An ACTH Stimulation Test is the most specific test for diagnosing adrenal insufficiency. Blood cortisol levels are measured before and after a synthetic form of adrenocorticotropic hormone (ACTH), a hormone secreted from the anterior pituitary, is given by injection.
As always, in health, Tanya x