It’s A Gut Feeling
In honour of IBS awareness month I wanted to turn the conversation back to this very important system - the Gastrointestinal System, that we fondly (or not so fondly if you suffer with IBS) call “The Gut”.
When assessing clients that come to see me with functional digestive disorders, rather than focus on what specific disease they may or may not have, I endeavour to assess and restore normal function across all the roles and processes within the system. If any of these go awry - IBS can be the result.
The most recognised symptoms are:
Pain and Cramping
Diarrhea
Constipation. ...
Alternating Constipation and Diarrhea. ...
Gas and Bloating. ...
Food Intolerances and sensitivities . ...
Fatigue and difficulty Sleeping.
It is one of the most common reasons for a visit to the GP. As many as one in eight people have symptoms of IBS at any one time and it is a condition that greatly impacts daily life, causing sufferers anxiety about eating out or even going out for fear of a flare in their symptoms.
Once serious pathology has been ruled out (hopefully) instead of digging deeper to identify the underlying cause(s), conventional medicine typically offers medications to suppress gut symptoms which prove to be not very effective.
But assessing the gut from a functional / root cause perspective can really get under the hood of where the fault lies. So, this circles me back to the functionality and process that occur with a “happy gut”, best broken down into 5 areas:
The 5 key roles of the digestive system
Digestion & absorption
Immune function & Oral Tolerance
The Gut microbiome
The maintenance of an immune barrier
The Nervous system of the gut
In this blog post over a year ago I spoke about the digestion and absorption element, so have a read over. Today I’d like to explain the gut microbiome in a little more detail, and show how if this goes array can easily cause “IBS”.
A healthy gut is associated with a diverse and balanced, stable, well-functioning microbial ecosystem within. It is now widely understood that disturbance of the complex equilibrium of the gut microbiota is associated with the development of various disorders, including metabolic (like weight gain or weight loss resistant), immunologic, digestive and even psychological/behavioural disorders. Disturbances or imbalances in gut microorganism communities are frequently referred to as “dysbiosis”.
What is Dysbiosis?
When the body and those pounds of non-human microbes living inside our guts (the gut microbiome) are in harmony, we are in SYMBIOSIS: a balanced, mutually beneficial relationship between us and those several hundred species of alien bugs. The gut, brain, and the rest of the body are in balance – in health, free from disease. In return for a pleasant home, these friendly organisms in our guts (often referred to as our old friends) allow us to thrive by:
Producing important biological chemicals like serotonin and dopamine (needed for brain function)
Synthesizing vitamins
Producing energy
Detoxifying the body
Inhibiting and killing off harmful bacteria and other nasty bugs
Maintaining a healthy immune system
Providing a protective coating on the bowel walls
Promoting normal peristaltic action in the bowel to keep us regular
But when, as happens too often, the harmonious relationship between the body and the large colony of bacteria, yeasts, viruses, parasites, etc living in our guts becomes out of balance, we are in DYSBIOSIS.
So what exactly can cause dysbiosis?…… it’s never one thing, but a combination of factors that over the years accumulate to disrupt the harmony of symbiosis. Here are the top causes I have researched and see playing out with clients that come to me for help:
A fibre and colour deficient diet: ie if you look at your plate and it’s predominantly white or beige
Antibiotics: The human microbiome is overly exposed to antibiotics, due, not only to their medical use, but also to their utilization in farm animals and crops. Microbiome composition can be rapidly altered by exposure to antibiotics
Other medications, such as The Oral Contraceptive pill: This study drew association Between Long-term Oral Contraceptive Use and Risk of Crohn’s Disease Complications in a nationwide study. It has also been established that birth control pills have an impact on the vaginal microbiome, as it is well documented that the pill increases the incidence of vaginal yeast infections
Infants born via C section birth
Infant formula instead of breast milk
Prolonged stress: high levels of cortisol and inflammatory molecules called cytokines disrupt the community of the gut microbiome and findings show that the stress hormone cortisol directly induces shifts in the gene expression profiles of the oral microbiome that reproduce results found in the profiles of expression of periodontal disease!
Chronic illness: any chronic illness will have a component of inflammation to the picture, and thus the point previously on the impact of cortisol plays out again.
High fat diets: even deemed “healthy” diets like Keto diets or using “healthy” fats like coconut oils excessively changes the microbiome towards more prevalence of sulphate reducing species. Hydrogen sulfide is the final product of sulfate-reducing bacteria metabolism. Its high concentration in the gut can adversely affect the bowel environment and intestinal microbiota - and voila: wind and gas and bloating.
Chemotherapy
Alcohol: causes “leaky gut” and dysbiosis.
Three Ways Dysbiosis Can Impact Your Gut
1. Too much of the “bad” overgrowing in the gut is the most basic imbalance. An overabundance of “bad,” typically inflammatory, bacteria, or too much yeast (candida albicans is a particularly common and unwelcome yeast in large amounts) are two examples of overgrowth that cause dysbiosis. An unwelcome virus or parasite can also cause overgrowth imbalance.
2. Microbial undergrowth can be the culprit. It is rarer than the situation above, but sometimes a stool test result shows an under-abundance of all bacteria – good and otherwise. An under-abundance indicates we need to work on improving the terrain (the gut lining) where the flora will take residence, as well as supporting the growth of the flora we want to encourage. We do this with probiotics, prebiotics, lining supportive supplements like glutamine, and healthy, bacteria-supportive foods.
3. Your microbiome settles in the wrong place. Living microbes are wanted, but we need them to live where they belong, and not take up residence in places where they cause problems. Most frequently, this type of dysbiosis is SIBO (Small Intestinal Bacterial Overgrowth). SIBO occurs when the gastrointestinal microbiome has shifted from primarily growing and thriving in the large intestines (the colon) to taking up residence in the small intestine in too great a number. This tends to cause digestive problems and bloating, but can be silent as well. Herbs and antibiotics are our go-to for treating SIBO.
Conditions Influenced by microbiome
“Poor gut health” might bring to mind intestinal and digestive disorders including inflammatory bowel disease, irritable bowel syndrome (IBS), and coeliac disease symptoms — but these are far from the only problems tied to dysbiosis. Studies show that dysbiosis of the microbiome is associated numerous disorders that affect us internally (which may not always be obvious) and externally (affecting us in more apparent ways, such as changing the appearance of our skin and body weight).
A lack of healthy gut bacteria is now tied to the onset of conditions like:
Food allergies
Digestive disorders - diagnosed IBS
Asthma
Diabetes
Arthritis
Fibromyalgia
Eczema and psoriasis
Metabolic syndrome, weight loss resistance and cardiovascular diseases
What to do?
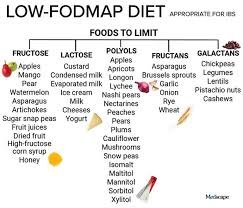
Because dysbiosis can fall into a number of categories there isn’t one diet that fits all I’m afraid. For example if you have the type of dysbiosis where microbes have over populated the small intestine - fermentable fibre is not your friend where as, if it’s an overgrowth of opportunistic bacteria in the colon then fibre is indeed what you need. This is why the low FODMAP approach (for a limited) period is helpful because it takes out highly fermentable carbohydrates.
FODMAP is a collection of naturally-occurring short-chain carbohydrates or sugars (only one or two sugars linked together), which the gut has trouble digesting in some people. FODMAP itself stands for Fermentable, Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
F stands for fermentable – and refers to indigestible carbohydrates producing gas. It’s a more general overview of symptom-causing foods.
Oligosaccharides – includes fructans and galacto-oligosaccharides (GOS) ( in foods like wheat, onion, garlic and beans)
Disaccharides –particularly means lactose (mostly in milk, soft cheese and ice cream)
Monosaccharides – pertains to fructose, often found in apples, pears and honey
And
Polyols – includes sugar alcohols, such as sorbitol and mannitol, which are found in some stone fruits (like peaches, apricots or cherries), veggies (like mushrooms) and gum.
Some general recommendations (please bear in mind everyone has a unique story and presentation so these are guidelines) would be:
70% of your diet and plate should be plant based
Fruit and vegetables are an excellent source of both soluble and insoluble fibre - avoiding FODMAPS - see chart
Try eating soups and stews, as these ensure your vegetables are well cooked and easy to digest, without losing valuable nutrients.
Introduce raw fruits and vegetables slowly, in small quantities and alongside other food.
Try peeling the fruits and vegetables you find problematic.
Remove wheat and it’s products such as biscuits, pasta, pizza
Remove milk, not all dairy products - just milk
20% should be quality protein
From oily fish like salmon, eggs, seafood, nuts, seeds and meat
10% should be healthy fats/oils and condiments
Herbal teas specifically camomile, liquorice and nettle are soothing and calming to the gut.
If I had to choose just one supplement product, I’d recommend IB pro: it contains lemon balm, chamomile and fennel seed which are traditionally used in western herbal medicine for their antispasmodic and carminative effects, flatulence and dyspepsia.
And ultimately find a health practitioner that can guide your through your bespoke journey to better digestive help.
I am thinking about putting an IBS 4-week self help course together to help suffers which would be delivered virtually - if this interests you, send me a thumbs up message.
In health, Tanya x